DOJ Sues Walgreens for Millions of Illegitimate Prescriptions Filled
Drug Topics
JANUARY 20, 2025
The lawsuit alleges Walgreens has been filling prescriptions in violation of the Controlled Substances Act since 2012.
This site uses cookies to improve your experience. To help us insure we adhere to various privacy regulations, please select your country/region of residence. If you do not select a country, we will assume you are from the United States. Select your Cookie Settings or view our Privacy Policy and Terms of Use.
Cookies and similar technologies are used on this website for proper function of the website, for tracking performance analytics and for marketing purposes. We and some of our third-party providers may use cookie data for various purposes. Please review the cookie settings below and choose your preference.
Used for the proper function of the website
Used for monitoring website traffic and interactions
Cookies and similar technologies are used on this website for proper function of the website, for tracking performance analytics and for marketing purposes. We and some of our third-party providers may use cookie data for various purposes. Please review the cookie settings below and choose your preference.
 Prescription Filling Related Topics
Prescription Filling Related Topics 
Drug Topics
JANUARY 20, 2025
The lawsuit alleges Walgreens has been filling prescriptions in violation of the Controlled Substances Act since 2012.

Drug Topics
NOVEMBER 14, 2022
Timing of treatment initiation is crucial for patients with cancer.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.

Pharmacy Times
JULY 28, 2023
Thousands more people filled their insulin prescriptions following the introduction of the cap in January 2023, especially compared to those who were not enrolled in Medicare, a new study finds.

Pharmacy Times
DECEMBER 4, 2023
The proportion of prescriptions by a 340B-affiliated physician increased from 9.4% in 2020, but the prescriptions filled by 340B pharmacies increased from 18.4% in 2013 to 19.3% to 49.9%.

STAT
JUNE 3, 2024
Paul Marchetti, the head of insurer Elevance Health’s pharmacy benefit manager, has left the company amid a wave of consumer complaints about patients receiving incorrect medicines or being unable to get their prescriptions filled.

Fierce Healthcare
JUNE 17, 2024
Uninsured consumers find the greatest savings, while Medicaid patients see none at all.
pharmaphorum
JULY 9, 2024
The six largest PBMs in the US manage nearly 95% of all prescriptions filled in the US, a “concentrated market structure” that has allowed them to “profit at the expense of patients and independent pharmacists,” according to the financial regulator.

STAT
APRIL 25, 2024
More than 90% of prescriptions filled that year were for generics or biosimilars, up from just over 18% the year that Hatch-Waxman was passed. The Hatch-Waxman Act of 1984, which gave rise to the modern generic drug market, was one of the most significant cost-reducing policy innovations of the last 40 years.

PharmExec
JANUARY 29, 2025
Prescription data between 2017 and 2023 revealed that while Adderall prescription fills decreased following the shortage, many children transitioned to alternative stimulants for attention-deficit/hyperactivity disorder.

Drug Store News
DECEMBER 5, 2023
In a recent podcast, Mark Cuban and Ferrin Williams address rebates, the need for transparency and talk about the future of prescription filling behavior.

IDStewardship
JUNE 6, 2023
Streamlined Prescription Filling : AI systems can automate prescription filling processes by extracting relevant information from electronic prescriptions, verifying insurance coverage, and generating labels. Faster and more accurate prescription filling leads to increased patient satisfaction.

STAT
AUGUST 17, 2023
But health care stocks fell significantly less than other companies as the amount of care received and prescriptions filled returned closer to pre-pandemic norms. By almost every measure, 2022 was a bad year for the stock market.

pharmaphorum
JANUARY 18, 2022
In 2008, CVS Caremark, a prescription benefit management company, signed on to use Microsoft’s HealthVault. Consumers could keep track of their prescriptions filled at CVS pharmacy or through Caremark and were able to save copies of their health records and share them with family members, physicians or third parties of their choice.

Digital Pharmacist
JULY 11, 2023
By providing regular check-ins, medication adjustments, and lifestyle advice, pharmacies can build long-term relationships with patients, resulting in increased prescription fills and customer loyalty.

The Checkup by Singlecare
JANUARY 20, 2023
An estimated 90% of prescriptions filled in the United States are for commonly prescribed generic drugs. Chances are, you’ve taken a generic or authorized generic medication, and for good reason—according to the U.S. Food and Drug Administration (FDA), generic medications cost 80%-85% less than brand-name drugs.

Digital Pharmacist
OCTOBER 26, 2023
Streamline Transfers : If your community is being impacted by retail chain closure, then there are likely many frustrated patients in your community who are in need of getting their prescriptions filled quickly.

The Checkup by Singlecare
JULY 2, 2024
Depending on where you get your prescription filled, though, the price can vary a lot. Without help from your health insurance plan, Medicare Part D, or Medicaid, you can expect to pay the typical retail price of $1,476 for a 28-day supply (a pack of four pens). The drug comes in six strengths: 2.5 mg, 5 mg, 7.5mg, 10 mg, 12.5

The Checkup by Singlecare
AUGUST 1, 2024
Your out-of-pocket costs depend on where you get your prescription filled as well. Research has determined that prescription drug prices can vary significantly between pharmacies, even ones in the same town. McKinney, MD, primary physician at Healthy Outlook.

The Checkup by Singlecare
APRIL 17, 2024
That price could depend on where you get your Mounjaro prescription filled, though. Without help from a health insurance plan, Medicare Part D, or Medicaid, the drug’s list price is $1,069.08 per 30-day supply (a pack of four pens).

The Checkup by Singlecare
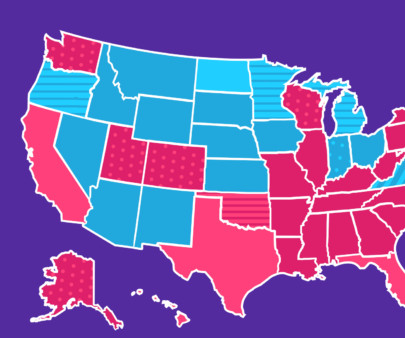
DECEMBER 5, 2023
The following list ranks the states that had the most Ozempic prescription fills at the pharmacy in 2023. Where is Ozempic most popular? Using SingleCare data, we have found the states where Ozempic is most popular.

The FDA Law Blog
DECEMBER 4, 2023
Within one month of each comprehensive review, the pharmacy must prepare a written report identifying prescriptions filled that were not issued for a legitimate medical purpose or filled outside the usual course of the professional practice of pharmacy, and prescriptions in violation of the permanent injunction terms.

The People's Pharmacy
JUNE 1, 2023
My own experience (after retirement) as a pharmacy customer: Why does it take so darn long to have a prescription filled? On a few occasions since retiring, I have had an antibiotic prescription filled (usually amoxicillin) for an abscessed tooth. I don’t take any medications myself on a regular basis.

The Checkup by Singlecare
JULY 3, 2024
Calling other pharmacies may help if you are having difficulty getting your prescription filled at your local pharmacy. A short supply of Adderall due to an Adderall shortage could also cause dosing disruptions.

DiversifyRx
APRIL 18, 2024
Have employees in their zone of genius position – your fastest typist inputting prescriptions. Prescription Fill Accuracy: Ensuring Patient Safety Accuracy is paramount when filling prescriptions in a pharmacy. Reduce phone calls with an IVR system.

PharmD Live
MAY 13, 2024
The Centers for Disease Control and Prevention notes a significant increase in prescriptions filled for American seniors from 1999 to 2012, enhancing the risks associated with medication use.

The Checkup by Singlecare
JULY 16, 2024
Then, you can choose to have your Mounjaro prescription filled at the pharmacy offering the lowest cost. Regularly checking prices ensures you’re getting the best deal possible.

The Checkup by Singlecare
JULY 17, 2024
Because you’ll receive more insulin per prescription, Toujeo Max Solostar also costs more than Toujeo Solostar. Each prescription fill includes 2, 3 ml pens and costs about $781 without insurance. ml of 300 units/ml pen $175 per 3, 1.5
The Checkup by Singlecare
MAY 29, 2024
What you need to know before buying Adderall online First things first: There is a difference between buying stimulant medication online without a prescription and getting a valid Adderall prescription filled online, says psychiatrist Sid Khurana , M.D., the medical director for Nevada Mental Health.

The Happy PharmD
DECEMBER 17, 2024
The convenience of receiving prescriptions at home is appealing, but its coming at a hidden cost. Over the past decade, mail order pharmacy sales have more than doubled, growing from $86 billion to over $206 billion, yet the number of prescriptions filled through mail order only increased by 11%.

The Checkup by Singlecare
JULY 2, 2024
After that, prescriptions filled with the card cost $25 or more. However, many plans require prior authorization and may only cover part of the cost of this drug. Also, if you’re eligible for the QSavings Card, you can get your first 30-day supply of Quviviq for free. Is there a cheaper alternative to Quviviq?

The Checkup by Singlecare
NOVEMBER 14, 2024
Have your prescription filled: Once the request is approved, you can pick up your prescription at your local pharmacy. This means your healthcare provider must submit a request to Medicaid explaining why Nurtec is necessary for your treatment.

Digital Pharmacist
JULY 3, 2023
Level of Liability Exposure : Evaluate the nature and extent of potential liability claims your pharmacy may face, such as errors in prescription filling or adverse drug reactions. Potential Loss Due to Business Interruption : Estimate the financial impact if your pharmacy temporarily ceases operations due to unexpected events.
Digital Pharmacist
DECEMBER 22, 2023
According to the NCPA 2023 Digest , 24 percent of pharmacies are currently using robotics for compliance packaging and it is anticipated that number will grow in 2024 and robotics will play an increasing role in prescription filling, reducing wait times, and enhancing medication management precision.

Digital Pharmacist
JULY 21, 2022
At this time patients are also unable to get all of their prescriptions filled from MCCPDC; they only offer certain medications at the moment and no controls are included. The personal care and connection one receives at an independent pharmacy will also be missing for the patients filling from MCCPDC.
The Checkup by Singlecare
DECEMBER 6, 2023
Thanks to our consistently low prices we tend to see trends in the medications that people fill at the pharmacy using our coupons. We compiled prescription fill data from the year to discover the 50 most popular medications from around the country. Read on to see if any of your prescriptions made the list.

The Checkup by Singlecare
NOVEMBER 6, 2024
It’s a good idea to check prices at different pharmacies and have your prescription filled at the one that’s most affordable. But this is an average cost, and several factors can influence what you pay: Dosage: If your healthcare provider prescribes a higher dose, it may cost more than lower doses.
The Checkup by Singlecare
SEPTEMBER 30, 2024
This could be time-consuming, so be sure to discuss interim treatment options to help manage your symptoms until you can get your prescription filled. Once the prior authorization is approved, take your prescription to a pharmacy that accepts Medicaid.

BuzzRx
FEBRUARY 3, 2023
In addition to denying prescriptions for emergency birth control pills and hormonal contraceptives, pharmacists in those states are not required to provide patients with an alternate route to have those prescriptions filled. Do I need a prescription for Plan B?

pharmaphorum
MAY 10, 2022
Hutnik shared a story from her experience where tracking community adoption of a therapy helped them to target more receptive communities, leading to prescription fills almost eight times higher. And I think this is well doable now.”. Advice for communicators.

The Checkup by Singlecare
SEPTEMBER 11, 2024
The total day supply available from a single prescription fill may exceed the duration prescribed. A tube of Tobradex ophthalmic ointment should last for a prescribed course of treatment for an eye infection, which generally does not exceed a 2-week course.

The Checkup by Singlecare
NOVEMBER 17, 2022
You can offer to transfer prescriptions from the patient’s other pharmacies and sync all prescription fill dates to cut down on visits to the pharmacy. . Having the patient use one pharmacy makes it easier to notice discrepancies in the patient’s medication profile. Update the patient’s medication list .

pharmaphorum
FEBRUARY 18, 2021
Between December 1, 2018 and January 31, 2019, 65% of erectile dysfunction prescriptions filled were for Viagra or its generic version 12. RESULT: Pfizer still holds a lead in the erectile dysfunction market even as generics erode sales. Prilosec – Benchmark for franchise management.

The Checkup by Singlecare
JANUARY 22, 2023
It is also possible to get CombiPatch or similar treatments at a reduced price through other options, such as a SingleCare prescription discount card. Eligible patients could pay less for prescription fills of CombiPatch. Use a manufacturer coupon The manufacturer of CombiPatch may offer a coupon or copay savings card.

The Happy PharmD
APRIL 26, 2023
But most pharmacies should be able to obtain it in a day or two if they need to fill a patient’s prescription especially since my girlfriend was a regular customer of this pharmacy. She has all her prescriptions filled at one particular pharmacy. She had it filled at another pharmacy. The directions were incorrect.
Expert insights. Personalized for you.
We have resent the email to
Are you sure you want to cancel your subscriptions?

Let's personalize your content